
Microtia is a congenital condition causing underdeveloped outer ears, often with middle ear deformities, while inner ear function remains intact. Affecting 0.83 to 17.4 per 10,000 births globally, it is more common in Hispanics, Asians, and Native Americans.
Microtia looks different for every child. Some babies with microtia are born with a slightly smaller ear, while others have no ear (anotia). The most commonly used grading system to describe microtia is shown below. The grade increases from 1 to 4 based on the severity of the condition.

Small, but almost normal ear

Small ear with some recognizable anatomy, canal may be normal or small

Small remnant of soft tissue with no ear canal
No external ear and no ear canal (Anotia)
We are MicrotiaMD, specializing in professional medical services for the reconstruction of ears for patients with congenital microtia and acquired external ear loss. The center is led by the internationally renowned reconstruction specialist, Professor Guo Shuzhong
Ear reconstruction surgery is best performed between the ages of 7 and 12. At this age, the child’s facial bones are sufficiently developed to ensure a good outcome, yet they are still young enough to achieve optimal results. Therefore, surgery can be considered when the child starts elementary school (around age 6), but the ideal age is between 7 and 12.
It’s best to schedule a consultation as early as possible, ideally 6 months or more in advance. This allows sufficient time for planning, preparation, and understanding the details of the surgery.
Whether the surgery can be reimbursed depends on local medical policies and the hospital’s reimbursement system. It’s a good idea to inquire with the hospital’s financial department during the consultation to see if reimbursement options, such as through insurance or government programs, are available.
If the ear deficiency is due to microtia (congenital ear deformity) and the ear canal is not fully developed, hearing may be affected. In many cases, children may need to wear a hearing aid to compensate for the hearing loss in that ear, especially if the ear canal is underdeveloped or closed.
If the child has facial asymmetry that needs to be addressed, it may be possible to treat it at the same time, depending on the specifics of the case. This can be discussed during the consultation to determine the best approach
The best time for the surgery is generally in the cooler months when the risk of infection and swelling is lower. After surgery, the ear will be carefully protected with bandages, and compression should be avoided to ensure proper healing and shape.
The ear reconstruction created through this surgery is designed to be permanent and will typically last a lifetime. However, periodic check-ups are recommended to ensure that the ear continues to maintain its appearance and functionality.
The success rate of ear reconstruction surgery is very high when performed by a skilled surgeon like Professor Guo, with many patients achieving excellent aesthetic results. The procedure has been refined over years, ensuring predictable outcomes.
The surgery involves using the child’s rib cartilage to reconstruct the ear. Cartilage is harvested from the rib area and then sculpted into the shape of a natural ear. The cartilage is then carefully implanted into the area where the ear is missing. The procedure is done with high precision to ensure the best aesthetic and functional result.
The cost of ear reconstruction surgery can vary depending on the specific case, but typically ranges in the tens of thousands of RMB. It’s recommended to confirm the cost with the hospital when you schedule a consultation.
Yes, Professor Guo Shuzhong, a leading expert in ear reconstruction, usually performs the surgery personally. Additionally, Doctor Shi Junli is also performing ear reconstruction surgeries. Both Doctor Shi and Professor Guo have extensive experience in this field, ensuring high-quality care and outcomes for patients.
As with any surgical procedure, there are risks involved, such as infection, scarring, loss of cartilage, or complications related to anesthesia. However, when performed by a skilled surgeon like Professor Guo, the risks are minimized.
Rib cartilage used for ear reconstruction does not absorb over time. It remains stable and continues to maintain its shape after being implanted.
In some cases, the ear canal can be opened simultaneously with ear reconstruction surgery. However, this depends on the specific situation and the development of the ear canal, which will be evaluated during the consultation.
Rib cartilage is commonly used for ear reconstruction, and it is usually taken from the child’s own rib. Taking rib cartilage does not significantly affect the child’s growth or development. While the removal of rib cartilage may cause some discomfort, it generally does not lead to chest collapse or affect mobility.
If you would like to know more, feel free to contact us via email:
gehao.zhang@ufh.com.cn

In most cases the cause of microtia CANNOT be determined. It is thought that microtia may occur due to a combination of environmental, genetic and other factors. It is important to understand that even though so many parents feel guilty that their baby was born with a birth defect, nothing a mother did during pregnancy caused the microtia.
Rarely, a single gene abnormality can cause microtia, as can exposure to a medicine called isotretinoin (Accutane®) during pregnancy. Recently the CDC found an increased risk for microtia in mothers who were diabetic before they became pregnant.

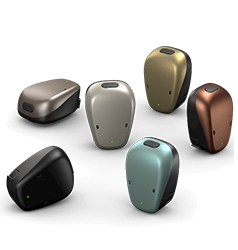



Aural Atresia is an underdeveloped external ear canal, eardrum and middle ear bones. It is often associated with microtia, a condition in which the outer ear is small, malformed or missing. Those with aural atresia most often have abnormalities of the outer and middle ear, but a normally functioning inner ear (cochlea) and hearing nerve. This condition results in a CONDUCTIVE hearing loss.

Small remnant of soft tissue with no ear canal

Small remnant of soft tissue with no ear canal
Aural atresia usually involves only one ear (unilateral atresia) and occurs in 1 in 10,000 to 20,000 births. Bilateral atresia, when both ears are affected, is much more rare. Children with aural atresia and one normal hearing ear may develop normal speech but have trouble knowing where sound comes from, referred to as “sound localization.” Regular appointments with an audiologist are important to confirm the child’s hearing isn’t changing in either ear.
Babies with bilateral atresia have significant hearing loss. Doctors recommend newborns use hearing aids to help develop speech and language.
Learn how sound is normally processed through the outer, middle and inner ear through this animated video.
Children with aural atresia have a conductive hearing loss with abnormal air conduction, but often have normal bone conduction. An audiogram is used to diagnose the type and severity of hearing loss. Learn about audiograms in this video.


Commonly known as BAHAs (Bone Anchored Hearing Aids) or BAHS (Bone Anchored Hearing Systems), these devices bypass the abnormal outer and middle ear by sending sound through the skull bone directly to the functioning inner ear. The BAHA can be worn on a softband, an adhesive sticker, a titanium abutment or magnetically. The softband or adhesive form can be worn starting in infancy; the titanium abutment and magnet can be surgically implanted when the skull is of proper thickness (approximately 6 years old). These four videos explain how each system works.




During PIER surgery, Dr. Lewin uses a scarless technique to surgically place the titanium implant into the skull. This eliminates the need for an additional surgery with general anesthesia after the microtia ear reconstruction. The type of surgical implant (abutment or magnet), brand of processor, and processor accessories are all chosen by the patient and their local audiologist.
Rarely, a single gene abnormality can cause microtia, as can exposure to a medicine called isotretinoin (Accutane®) during pregnancy. Recently the CDC found an increased risk for microtia in mothers who were diabetic before they became pregnant.
Children may become aware of their own facial differences as early as two to three years of age. Although not always the case, microtia can have a significant psychological impact on children and their families. This is especially important to be aware of when children with microtia attend school as they may experience more teasing, and even bullying, from their peers. Several published studies on the psychological effect of microtia have found:
Increased difficulty in social integration and lack of self confidence for children with microtia.
Mood disorders increase with age in microtia patients who have not had reconstructive surgery.
Teasing from peers and the emotional impact on parents were risk factors for depression, social difficulties and aggression.
A higher prevalence of interpersonal sensitivity, depression and anxiety are seen in mothers of children with microtia.
Ear reconstruction has a significant psychosocial benefit to the majority of patients.

Despite these studies, parents should know there are ways to minimize potential negative psychological effects. Many experts believe a parent’s attitude toward their child’s microtia is the most important factor in the psychological health of the child.


Dr. Shuzhong Guo is a distinguished expert in reconstructive and plastic surgery, known for his pioneering work in craniofacial surgery, including ear reconstruction. Dr. Guo has served as a professor at the Fourth Military Medical University and led groundbreaking procedures, such as the first face transplant in Asia. His innovative use of techniques like tissue expansion and cartilage sculpting for microtia has set new standards in the field. Children undergoing early reconstructive surgeries under Dr. Guo’s care have shown remarkable psychological resilience, with parents often noting immediate boosts in their child’s self-confidence post-surgery. “We sometimes forget our child was born with a small ear,” is a common reflection shared by families after the successful outcomes of Dr. Guo’s work.
